NDSU Researcher Studies Disease-causing Bacteria
(Click an image below to view a high-resolution image that can be downloaded)
You can’t see them, but bacteria can cause serious health problems in the human body and on surfaces such as medical devices and food processing equipment.
The bacteria may show up as plaque on teeth or cause otitis, a middle-ear infection, or cystic fibrosis, a disease that causes thick, sticky mucus to build up in the lungs. The bacteria also can lead to a sometimes deadly foodborne illness.
These collections of bacteria, called bacterial biofilms, are the subject of intensive research in North Dakota State University’s Department of Veterinary and Microbiological Sciences.
An estimated 60 to 80 percent of bacterial infectious diseases involve the formation of biofilms, according to the National Institutes of Health and Centers for Disease Control and Prevention. Also, 76 million Americans suffer from foodborne illness each year.
Researchers don’t know how many of these foodborne illness incidents involve bacterial biofilms.
“However, food processing equipment is often contaminated with bacterial biofilms,” says assistant professor Birgit Pruess, whose lab is focusing on studying biofilms. “This is of particular importance in a state like North Dakota, where so much of our nation’s and world’s food supply is being produced.”
Pruess is one of a group of scientists in the Department of Veterinary and Microbiological Sciences conducting research on the development of infectious diseases and how organisms’ immune systems respond to those diseases. They are committed to understanding microorganisms and the disease process to enhance North Dakota’s efforts to protect against intentional and unintentional disease outbreaks.
But bacteria’s ability to form biofilm isn’t all bad: It can be used in bioindustrial processes. For instance, bioethanol production sometimes involves the formation of biofilm. This can be an advantage because the multiple species that form the biofilm are very close to each other, which facilitates the separation of the final products.
“The information that will be obtained from the research in my lab will constitute a major breakthrough in our understanding of the physiology that underlies biofilm formation and will have implications in several biofilm-associated problems and/or applications,” Pruess says.
One possible application is the development of novel drugs to treat biofilm-associated infectious diseases. Bacteria in a biofilm have a community lifestyle that has similarities to humans. They communicate with each other, are able to move to more desirable places and even have a molecular form of a memory that lasts about 20 seconds.
“As a general rule, disrupting the communication pathways that lead to processes like biofilm formation is a promising alternative to traditional drug therapies that reduce bacterial growth while inducing resistance,” says Pruess, whose lab has a long history of studying regulatory pathways at the genetic level.
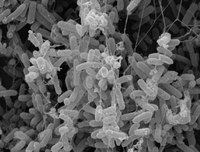
Biofilm-bound bacteria form three-dimensional structures consisting of multiple layers of bacteria. For example, bacteria at the outermost edge of the 3-D structure are exposed to more nutrients and oxygen than the bacteria in the center of the colony. The outermost bacteria also are exposed to the host’s immune system or, in cases of infectious diseases, antibiotics.
“Drugs are often unable to penetrate deep into the biofilm,” Pruess says. “This means that they will need a target at the surface of the 3-D structure that constitutes the biofilm. We anticipate that this project will lead to the identification of a number of genes that can serve as targets for novel biofilm prevention and treatment options.”
Her research aimed at identifying such surface targets is funded by a $358,750 grant from the National Institutes of Health.
A second project she is working on deals with determining the precise conditions under which bacterial biofilms form. Despite years of research on biofilms, few comprehensive studies address this question.
Pruess, in collaboration with Anne Denton, an associate professor in NDSU’s Department of Computer Sciences, found that nutrients available to the bacteria are instrumental in determining the amount of biofilm that is formed. Pruess and Denton will pinpoint single nutrients that will inhibit biofilm formation, which also will be helpful in developing biofilm prevention and treatment techniques.
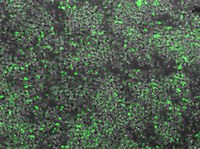
Pruess and Preeti Sule, a Ph.D. student, have studied a pathogenic E. coli strain grown on the surface of meat. E. coli is a naturally occurring bacterium found in the lower intestine of warm-blooded organisms. Most strains are harmless, but some can cause serious illness in humans.
The strain Pruess and Sule studied would not form biofilm under most laboratory conditions. However, it probably does when grown on meat, Pruess says.
They also found that eliminating flagella, the hairlike structures that help bacteria move, increased the bacteria’s ability to form biofilm, as well as the bacteria’s cell division rate and pathogenicity, or ability to produce an infectious disease in an organism.
“These findings open countless avenues to the development of novel meat treatments that would simultaneously reduce the cell number, the ability to form biofilm and pathogenicity,” Pruess says. “The research, which is funded by the State Board of Research and Education and the North Dakota Beef Commission, could help with one of the unresolved problems in meat processing: contamination with E. coli.”
NDSU Agriculture Communication - April 29, 2011
| Source: | Birgit Pruess, (701) 231-7848, birgit.pruess@ndsu.edu |
|---|---|
| Editor: | Ellen Crawford, (701) 231-5391, ellen.crawford@ndsu.edu |